Background
The frontline treatment of patients with symptomatic mantle cell lymphoma (MCL) requiring treatment varies in practice. In Ontario, Canada, transplant-eligible (TE) patients have been treated with chemoimmunotherapy followed by autologous stem cell transplant (ASCT). In 2013, R-CHOP alternating with R-DHAP prior to ASCT replaced R-CHOP alone as standard of care based on the European MCL Younger trial (Hermine JCO 2022). Although this regimen improves progression-free survival, there remains concern about its toxicity.
For transplant-ineligible (TI) patients, the standard of care has evolved over time. Evidence in support of bendamustine-rituximab (BR) efficacy in indolent lymphoma resulted in its increased use in TI patients with MCL over the last decade. However, real-world data are lacking on toxicities of this regimen compared to other chemoimmunotherapy. We aimed to characterize survival and healthcare utilization outcomes of patients with MCL using current treatment approaches.
Methods
We conducted a retrospective population-based study of patients with MCL using healthcare administrative databases from Ontario, Canada, from 2005 to 2020. Patients were defined as TE if they were less than 70 years old at the time of treatment initiation, and received either R-CHOP or R-CHOP/R-DHAP. Patients were defined as TI if they were 70 years or greater at the time of treatment initiation, and treated with BR or other forms of chemoimmunotherapy. The primary outcome was 5-year overall survival (OS), from the time of first treatment to death or end of the study period. Secondary outcomes were toxicities of treatment and healthcare utilization. Cox regression analyses were used to assess the impact of demographic and treatment variables on OS.
Results
A total of 918 patients with MCL were included in this study; 426 were TE and 492 TI.
For TE patients, 254 were treated with R-CHOP, and 172 with R-CHOP/R-DHAP. The median age of patients in both groups was 60 years (range 36-70 years, p=0.37). Patients treated with R-CHOP alone were followed for a mean of 6.01 years, and patients treated with R-CHOP/R-DHAP for a mean of 3.38 years. Maintenance rituximab (MR) was used in 70.5% of patients treated with R-CHOP and 77.3% of patients treated with R-CHOP/R-DHAP (p=0.12). ASCT was received by 53.5% of patients treated with R-CHOP and 83.7% of patients treated with R-CHOP/R-DHAP (p<0.01).
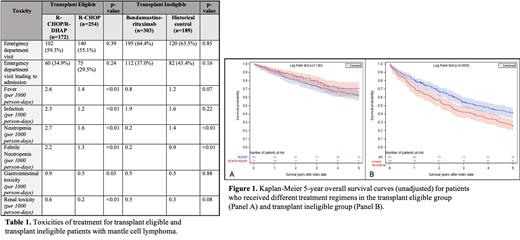
5-year OS of patients treated with R-CHOP/R-DHAP was 70.5% vs 62.0% for patients treated with R-CHOP regardless of transplant status ( Figure 1A hazard ratio [HR] 0.75, 95% CI 0.51-1.10). Of the 270 patients who received ASCT within 1 year of treatment initiation, survival was not impacted by prior receipt of R-CHOP alone or R-CHOP/R-DHAP (HR for R-CHOP/R-DHAP vs. R-CHOP 0.76, 95% CI 0.42-1.39). A higher proportion of patients treated with R-CHOP/R-DHAP required hospital admissions for fever, infection, neutropenia, and renal toxicity, compared to R-CHOP alone ( Table 1). There was no difference between regimens in the number of patients requiring emergency department (ED) visits between regimens (p=0.39).
492 TI patients were included; 303 treated with BR and 189 treated with other regimens, most commonly R-CHOP (n=62) or R-CVP (n=108). The median age of patients in both groups was 77 years (range 71-94 years, p=0.17), and there was no significant difference in comorbidities (p=0.23). MR was more commonly used after BR compared to historical regimens (72.6% vs. 54.5%, p<0.01).
5-year unadjusted OS of patients treated with BR was 40.3% and 27.5% for patients treated with R-CHOP/R-CVP ( Figure 1B), with significantly lower mortality with the use of BR (HR 0.68, 95% CI 0.51-0.89). After adjusting for age, sex, comorbidities, and MR, this was no longer significant (HR 0.86, 95% CI 0.65-1.14). MR use was associated with significantly lower mortality (HR 0.33, 95% CI 0.24-0.44). More patients treated with BR had hospital admissions for neutropenia and febrile neutropenia ( Table 1).
Conclusion
In this large population-based study of patients with MCL, R-CHOP/R-DHAP prior to ASCT showed a trend toward improved 5-year OS, though not significant. For TI patients, BR resulted in superior OS compared to other regimens with similar rates of toxicities, however this was not significant after adjusting for use of MR, suggesting other regimens followed by MR may be a reasonable alternatives.
Disclosures
Prica:Abbvie: Honoraria; Astra-Zeneca: Honoraria; Kite Gilead: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal